I've decided to write about it here because Ivor, in his magpie style, has scooped it up and dumped it where all can see, with a suitable explanation for those already in the know, but I think it will benefit from additional commentary.
Diet studies show LCHF is especially good for lowering fasting triglycerides and raising HDL, improving the TG/HDL ratio. Other diets are better for lowering LDL.
These are called surrogate endpoints; people don't usually die during weight loss trials (fat modification trials, usually with bigger numbers, are another story). If the diet lowers a "bad" marker or raises a "good" one, that is, markers such as lipids, blood pressure, BMI or HbA1c that are clearly associated with risk and easy to measure, that counts as success. These trials are too difficult and expensive to take much further than that (e.g. till people start dying).
The problem with this approach was vividly and disastrously demonstrated by the US Navy during World War Two.
If you're a US submariner firing a torpedo at a Japanese ship using a contact detonator and a shallow depth setting so it won't miss by running under the target, you'll most likely put a hole in that ship if you hit it, but you may not cause enough structural damage to sink it, and in underwater warfare you might not get a second shot (the Imperial Japanese Navy didn't really have this problem as their torpedoes were bigger and faster than the US equivalent).
The best way to optimize kills is to set the torpedoes to run deep, then explode them using a magnetic trigger that's detonated by passing under the ship's magnetic field. The consequent increased pressure from a proximal explosion in deep water will do more damage and hopefully break the ships back, allowing more ships to be sunk with the limited torpedo supply a submarine can carry on a long Pacific cruise. That's the theory, and the magnetic trigger was developed for the Mark 14 torpedo. Submariners were ordered to use it instead of the contact fuse.
Torpedo after torpedo fired at carefully set-up Japanese targets failed to explode. Boats that would later in the war devastate the Japanese merchant marine and Navy came back from patrol empty handed, their officers accused of cowardice or incompetence. The technology isn't flawed, you're just doing it wrong. The tide was eventually turned by submarine captains breaking orders, removing the magnetic triggers and changing the depth settings, to a predictable, indeed familiar, chorus of outrage and threats.
The Mk 14 torpedo still wasn't perfect (the contact trigger didn't work if it hit the target full-on, the depth setting mechanism was wonky, and so on) but the Japanese started to lose tonnage and the war.
The problem was that the expensive Mk 14 torpedo was developed during the Great Depression by a Navy operating on a minute budget. Habits of parsimony thus learned were continued into wartime.
The Mk 14 torpedo was never tested to detonation in any trial. If it ran deep enough under the dummy targets, and it had a magnetic trigger attached, or if it hit the target with a contact trigger attached, the trial was counted as a success.
In medicine this is called a surrogate endpoint.
And people are rightly sceptical about surrogate endpoints. Any line of evidence that gives new information about their reliability as predictors of death and disease is always welcome.
The evidence Ivor found concerns 3 lipid markers at baseline. They're not products of an intervention; they relate to diet, genetics, and metabolic health.
LDL, as we know, is raised by some of the saturated fats and lowered when these are replaced by other sources of energy.
TG is elevated (except in very low fat diets) in response to dietary carbohydrate.
HDL is raised by the same saturated fats that raise LDL, and is lowered by chronically elevated insulin levels such as we will see in insulin resistance and the early-to-middle phases of type 2 diabetes.
Someone who is metabolically healthy but eating a high-carbohydrate diet will have high TG, but because their insulin level is normal their HDL will not be depressed, thus the TG/HDL ratio will tend to stay in the normal range. In someone who is hyperinsulinaemic, TG on a high-carbohydrate diet may be even higher, and HDL will be depressed, creating an unfavourable TG/HDL ratio.
Excess insulin (or excess alcohol) will also increase production of unhelpful HDL subtypes, and high carbohydrate will make the LDL subtypes more atherogenic.
Dietary carbohydrate is thus the driver of this type of dyslipidemia, but is it necessarily worse than the high-LDL dyslipidemia that statins target?
The evidence from the trials:
The first set of graph is from a fibrate trial. Fibrates mainly lower TG/HDL, plus have nasty side effects. The black bars are the people who didn't get the drugs. That's who we're interested in in all these papers. HDL (cut-off 1.08) and TG (cut-off 2.3) correlate strongly with events. LDL (cut-off 5 - very generous!) is barely significant.
http://circ.ahajournals.org/content/85/1/37.long
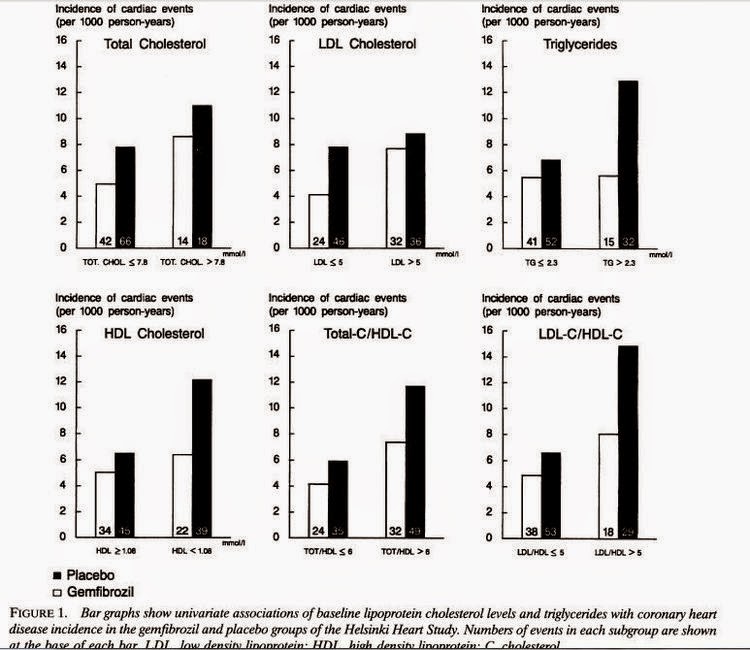
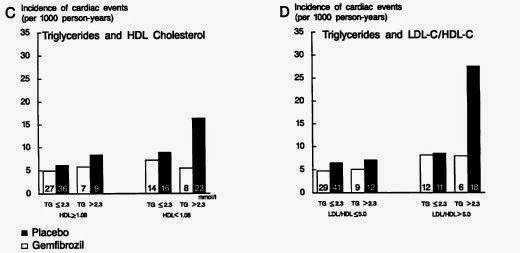
The second set of graphs, from the same trial, shows that high TG is a lesser risk factor in people with higher HDL, and that a high LDL/HDL ratio is especially bad if you have high TG. Despite the lower white bars everywhere (those treated with gemfibrozil had fewer cardiac events) "there was no difference between the [treated and untreated] groups in the total death rate."
The third graph, from a 2013 statin trial, shows that people in the highest quartile for HDL who don't get statins (which did work for others) but get placebo instead do better than anyone taking statins.
http://www.ncbi.nlm.nih.gov/pubmed/23948286

I also found this drug and non-drug study: note cut-off for LDL is now half what it was in the Gemfibrozil study. This shows how much fashions can change in 25 years, but makes no difference to the results.

