 |
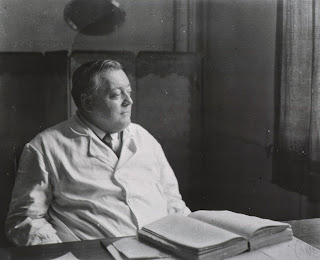
| Karl Petren 1868-1927 |
It is pretty well-accepted now that nutritional ketosis and diabetic ketoacidosis are quite different things, but it is not yet understood how nutritional ketosis prevents diabetic ketoacidosis. That it does so was clear in 1923; both Newbugh and Marsh[1] and Karl Petren[2] reported in that year from their respective diabetes clinics that a diet high in fat, restricted in protein, and very low in carbohydrate, fed to diabetic patients, including (certainly in the case of Newburgh and Marsh) those with juvenile-onset, or type 1 diabetes, prior to the introduction of insulin, resulted in no cases of DKA developing. Newburgh and Marsh also reported DKA developing in a fasting case, so the inhibition of DKA was not a result of carbohydrate restriction alone.
DKA is the result of the unrestrained action of glucagon, which stimulates lipolysis and proteolysis, flooding the liver with substrates for ketogenesis (fat and ketogenic amino acids) and gluconeogenesis (glycerol and glucogenic amino acids), in the absence of insulin. Glucose, in the absence of insulin, is also a glucogenic substrate and increases both glucagon release and hepatic gluconeogenesis. The combination of hyperglycaemia and hyperketonaemia that ensues produces a loss of fluid volume and a life-threatening acidosis.
How might feeding fat prevent this?
Raphi Sirt, in response to my restatement of this question recently, tweeted a paper that cited another paper referring to a 1970’s experiment in which people with insulin-dependent diabetes were withdrawn off insulin and given a peptide called somatostatin by researchers happily free from modern ethics committee constraints.[3] This hormone prevented DKA by inhibiting glucagon release from the pancreatic alpha-cells. Somatostatin exists in two main forms in human metabolism, as 14 and 28 length peptides, and somatostatin 28 is released from the delta cells of the gut and pancreas proportionately in response to the ingestion of fat; there is a partial response to protein and no response to carbohydrate, making the somatostatin 28 ratio of macronutrients the inverse of the insulin ratio.[4]
In normal metabolism somatostatin inhibits both insulin and glucagon release. It is probably responsible for mediating the slower digestive response needed when fat is consumed in a meal. But if you have no insulin to begin with, somatostatin is just a glucagon inhibitor. If you have too much insulin and low insulin sensitivity (and hence too much hepatic glucagon activity) it’s probably helpful too, as long as you aren’t also eating carbohydrate.
Unusually I could not find full-text version of references 3 and 4, so there are still some very unanswered questions. Did Gerich et al. know of the findings of Newburgh and Marsh in designing their experiment? What was the form of somatostatin they used? And, did the serum concentrations of somatostatin approximate those that might be attained with high fat feeding? If not, does the paracrine release of somatostatin 28 that inhibits glucagon necessarily result in such high serum levels?
All your help, as always, is appreciated.
[1] Further observations on the use of a high fat diet in diabetes mellitus. Newburgh LH and Marsh PL. Archives of Internal Medicine April 1923 Vol. 31 No. 4.
[2] Über Eiweissbeschränkung in der Behandlung des Diabetes gravis, Petren K, 1923 - On protein restriction in the treatment of diabetes gravis. Cited in: A Substance in Animal Tissues which stimulates Ketone-Body Excretion, Stewart FB and Young HG, Nature 1952; 170, 976 - 977 doi:10.1038/170976b0
[3] Prevention of Human Diabetic Ketoacidosis by Somatostatin — Evidence for an Essential Role of Glucagon. Gerich JE, Lorenzi M, Bier DM et al. N Engl J Med 1975; 292:985-989. DOI: 10.1056/NEJM197505082921901
[4] Effect of ingested carbohydrate, fat, and protein on the release of somatostatin-28 in humans. Ensinck JW, Vogel RE, Laschansky EC, Francis BH. Gastroenterology 1990 Mar;98(3):633-8